Appendicitis
Appendicitis is an inflammation of the ileocecal appendix, usually secondary to luminal obstruction. It affects 5% of the population and represents the most common abdominal surgical emergency. While it can occur at any age, there is a slight predominance in adolescents and young adults. Any clinical suspicion of appendicitis warrants referral to an emergency department for evaluation.
Its course is typically acute, and the existence of chronic appendicitis remains controversial.
Pathophysiology and Etiologies
Appendicitis results from the development of an infection, usually polybacterial, often due to increased luminal pressure secondary to obstruction caused by one of the following etiologies:
- Lymphoid hyperplasia in the submucosa +++
- Fecalith, foreign body, mucous plug
- Wall hypertrophy in inflammatory colitis (more frequently in Crohn's than in ulcerative colitis)
- Granuloma formation in parasitosis (Enterobius vermicularis, ascaris,...)
- Various: yersiniosis, tuberculosis, sarcoidosis, typhoid fever, amoebiasis, pinworm infection, measles, Epstein-Barr Virus (EBV), cytomegalovirus (CMV), tumors (carcinoid tumor in ~0.5% of surgical specimens), (sub)-occlusion,...
Exceptionally, the infectious origin can be hematogenous.
Clinical Presentation
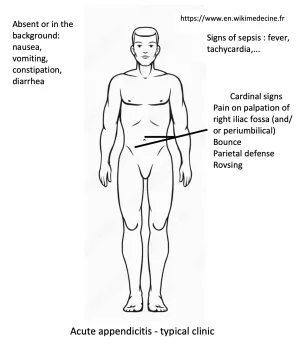
The typical symptomatology includes:
- Pain (100%) in the right iliac fossa (may start in the epigastric or peri-umbilical region and then migrate), severe and continuous, with rapid worsening. Radiation is exceptional.
- Functional disturbances: vomiting (30%), constipation (30%), diarrhea (30%)
- (Sub)fever (50%): 37.5-39.5°C, generally with mild tachycardia
The typical signs found on clinical examination are:
- Pain on palpation of the right iliac fossa, rebound tenderness in the right iliac fossa (very evocative), Rovsing sign (pain in the right iliac fossa when compressing the left iliac fossa... diagnostic value, however, debated...)
- Almost constant parietal guarding if the appendix is lateral-cecal.
- Pain on pelvic palpation
However, "atypical" presentations are not uncommon:
- Pelvic appendicitis:
- Hypogastric pain
- Dysuria, pollakiuria, tenesmus, diarrhea, false urges
- Main differential diagnoses: diverticulitis, pyosalpinx, testicular torsion, gynecological pathologies,...
- Retro-cecal appendicitis:
- Lower back pain or in the right iliac crest, psoitis (spontaneous flexion of the thigh with painful extension)
- Main differential diagnoses: kidney colic, pyelonephritis
- Sub-hepatic appendicitis: acute cholecystitis picture (abdominal ultrasound will correct the diagnosis)
- Meso-coeliac appendicitis: febrile small bowel obstruction picture (CT scan will correct the diagnosis)
- Herniated appendicitis: strangulated hernia picture (ultrasound will correct the diagnosis)
- Left-sided appendicitis mimicking sigmoid diverticulitis in cases of situs inversus (CT scan will correct the diagnosis)
- In children and the elderly, clinical presentation is frequently atypical (pain is more frequently diffuse,...)
Investigations
The diagnosis is generally clinical. Traditionally, additional examinations are only justified in cases of clinical doubt or for pre-operative assessment; a typical clinical presentation is sufficient to indicate surgery. The use of radiological imaging, however, tends to become more common, primarily for medicolegal protection purposes. It has not been demonstrated that this approach benefits patients. In any case, there is no justification for postponing exploratory surgery in cases of typical and severe clinical presentation.
- Biology: moderate leukocytosis (85%) with neutrophils (75%), elevated CRP (95%)
- Negative predictive value ~ 98% for normal leukocytes and CRP... but low positive predictive value.
- Abdomino-pelvic ultrasound: sensitivity varies from 30 to 90% depending on the forms, and specificity from 85 to 100%. It is especially useful for differential diagnosis and represents an alternative to be preferred over CT scanning in children, pregnant women, and thin subjects.
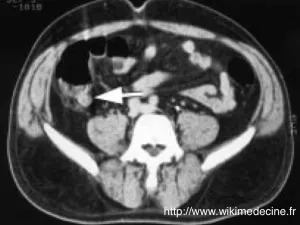
- Abdomino-pelvic CT scan with contrast injection: Positive predictive value of 98%. It has become the gold standard for diagnosis; in any case, it is indispensable in cases of diagnostic doubt.
- Abdomino-pelvic MRI: Positive and negative predictive values similar to those of CT scan. Non-irradiating but rarely used (cost and lack of availability). Used in practice for pregnant women in case of non-contributory ultrasound.
- Various examinations depending on the differential diagnoses considered (urine examination, pregnancy test,...)
Differential Diagnosis
See detailed article: Acute Abdominal Pain
The differential diagnosis is that of abdominal pain, to be adjusted according to the clinical expression. The main potential confusions are kidney colic, annexial pathologies, mesenteric adenitis, acute pyelonephritis, appendagitis, epiploic torsion, functional colopathies.
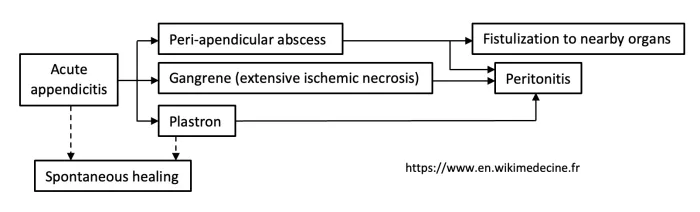
Natural Course and Complications
Catarrhal appendicitis is a form limited to the involvement of the (sub)-mucosa. Its possible progression to spontaneous healing or chronicity remains debated. The next stage is ulcerative appendicitis, which can progress to abscess formation, gangrene, the formation of an adhesion or peritonitis.
The main complications to look for are:
- Abscess formation
- Fistulization to neighboring organs
- Gangrene
- Generalized peritonitis due to:
- Appendicular perforation
- Bacterial spread
- Extensive gangrene
- Rupture of a peri-appendicular abscess
- Various (rare): septic "metastases," suppurative thrombosis of the portal vein, septic shock
Therapeutic Management - Treatments
Reference Treatment:
- General measures (anti-ulcer prophylaxis [e.g., ranitidine 150 mg/day], adapted analgesia [e.g., paracetamol 3 x 1 g/day +- tramadol 3 x 50 mg/day],...) and supportive care
- Preoperative preparation 1-3 hours: IV rehydration 2 to 3 l/24 hours, nasogastric tube aspiration in case of occlusion
- Antibiotherapy:
- Prophylactic if uncomplicated appendicitis.
- E.g., amoxicillin (2 g) - clavulanate (200 mg) 1 x IV
- To be administered within the hour preceding the intervention
- Curative for > 48 hours if intraoperative discovery of suppurative, gangrenous, perforated appendicitis, or peritonitis.
- E.g., amoxicillin (2 g) - clavulanate (200 mg) 3 x/day IV (in case of penicillin allergy: metronidazole 3 x 500 mg + ciprofloxacin 2 x 400 mg IV/PO). To be adjusted according to the results of intraoperative sampling.
- Emergency laparoscopic appendectomy (to be delayed in case of adhesion or clinical progression for several days). Resorting to laparotomy becomes the exception.
Antibiotic therapy alone as a first-line treatment is still debated. While seemingly as effective as surgery, it would lead to a high recurrence rate (up to 40%)... it remains in the realm of study or to be proposed to patients refusing the intervention...
And "chronic" appendicitis?
The possible evolution from catarrhal appendicitis regressing spontaneously to chronic appendicitis is discussed (given the limited success of appendectomies performed for this indication → are these possibly misdiagnosed cases of functional colopathies of the right iliac fossa?). In any case, various forms of chronic appendicitis have been described (atrophic chronic appendicitis, obliterative chronic appendicitis), generally interpreted as involutions of the appendix in the elderly or the evolution of minimal congenital malformations.
Bibliographie
Hawkey CJ et al., Textbook of clinical Gastroenterology and Hepatology, 2d edition, Wiley-BlackWell, 2012
Martin RF et al., Acute appendicitis in adults : Clinical manifestations and differential diagnosis, UpToDate, 2016
Martin RF et al., Acute appendicitis in adults : Diagnostic evaluation, UpToDate, 2016
Rohr S et al., Appendicite aiguë, EMC, Elselvier, Paris, 1999
Smink D et al., Management of acute appendicitis in adults, UpToDate, 2017