Respiratory function testing (RFT) - elements of interpretation
Last edited on : 22/09/2024
Respiratory function testing (RFT) study respiratory function, essentially through the study of respiratory volumes and flows and gas exchanges at rest and during exercise.
Although dependent on the patient's cooperation, respiratory function tests are one of the main examinations contributing to the development and follow-up of chronic dyspnea. The aim of this article is not to be exhaustive, but to provide all doctors, whatever their specialty, with the information they need.
Lung volumes
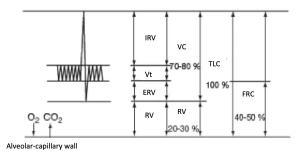
Lung volumes are measured by spirometry (measurement of mobilizable volumes) and inert gas dilution or plethysmography (measurement of inert volumes). These measurements are highly sensitive, and can be used to differentiate :
- Obstructive pathologies :
- Increased TLC and RV
- Increased RV / TLC ratio
- Restrictive pathologies:
- TLC decreased to < 80% of predicted value
- Increased RV / TLC ratio
- RV variable according to pathology
Airflow resistances
Airway resistance is determined by measuring forced expiratory and inspiratory volumes as a function of time using a spirometer. The results are usually presented as two curves:
Measurement of the Tiffeneau ratio (FEV1/FVC) and the morphology of the flow-volume curves can be used to differentiate between :
- Obstructive pathologies :
- Decreased FEV1 with Tiffeneau < 0.7 (according to GOLD criteria - does not recognize very distal obstructive disease).
- An abnormally concave expiratory flow-volume curve (reduced expiratory flow at low volumes). In the most severe cases of obstruction, PEF will also be lower than predicted.
- In geriatric patients, a curve characterizing mild obstruction should be considered physiological.
- Note that in cases of obstruction of the upper airways (larynx, trachea) or sometimes of the bronchial tubes, a "plateau" curve may be observed.
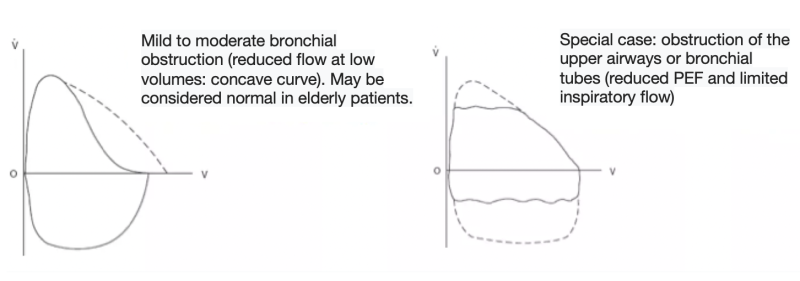
- Restrictive pathologies
- Decreased FEV1 with Tiffeneau > 0.7 (proportional decrease in FVC). Tiffeneau > 1.1 suggests pulmonary fibrosis.
- The flow-volume curve is a "reduced model" of the normal curve: all predicted values are decreased in a relatively harmonious way, so the slopes are preserved (decrease in expiratory and inspiratory flows for all volumes).
Reversibility test in an obstructive syndrome
An important step in the development of an obstructive syndrome is to determine whether it is (partially) reversible to the administration of a bronchodilator. Reversibility is defined as an improvement in FEV1 or FVC > 12% and 200 ml ten minutes after administration. In this case, if Tiffeneau remains < 0.7, partial reversibility is assumed.
If the test is negative, it is useful to repeat it at follow-up EFR (susceptibility to bronchodilators varies over time → many false negatives). Administration of long-acting bronchodilators in the hours preceding the test is a frequent cause of false negatives.
Respiratory syndromes
Restrictive syndromes
EFR characteristics :
- TLC and VC decreased with TLC < 80%.
- FEV1 and FVC reduced with Tiffeneau > 0.7
Etiologies :
- Chest wall involvement :
- Bone involvement :
- Scoliosis, ankylosing spondylitis, funnel chest, abdominal obesity, pleural damage, cardiomegaly, abundant ascites, diaphragmatic hernias
- Neuromuscular disorders:
- diaphragmatic disorders, spinal lesions, hemiplegia, poliomyelitis, muscular dystrophies, myopathies, amyotrophic lateral sclerosis, Guillain-Barré, myasthenia, Lambert-Eaton, botulism
- Bone involvement :
- Parenchymal involvement :
- Lobar or pulmonary excision, atelectasis, pneumonia, pulmonary edema, interstitial lung disease, pulmonary fibrosis, pneumoconiosis, alveolar proteinosis, tuberculosis sequelae
Obstructive syndromes
EFR characteristics :
- Tiffeneau decreased < 0.7
- FEV1 and VC decreased. FEV1 value reflects syndrome severity (mild if > 50%, moderate if 35-49%, severe if < 35%).
- FRC increased in severe cases. TLC is > 80%.
- Note that in cases of obstructive distal airway disease (= "small airway syndrome") (e.g., early onset in smokers), Tiffeneau may still be normal. However, the flow-volume curve will be concave (to be compared with the patient's age) and the MPEF 25-75 (median peak expiratory flow) < 60% and the MPEF 25 and 50 decreased.
Etiologies of bronchial obstructive syndromes :
- Non- or poorly reversible :
- Chronic obstructive pulmonary disease (COPD)
- Chronic bronchiolitis
- Bronchiectasis
- Cystic fibrosis
- Ciliary dyskinesia
- Reversible :
- Asthma
Mixed syndromes
Defined by the coexistence of a Tiffeneau < 0.7 and a TLC < 80%.
They are frequently encountered in certain specific pathologies (bronchiectasis, pneumoconiosis, sequelae of tuberculosis, sarcoidosis, etc.) and in the combination of the above-mentioned pathologies.
Diffusion capacity (Dlco) = transfer factor (Tlco)
Diffusion capacity (Dlco) or transfer factor (Tlco) is a measure of the lung's gas exchange capacity (normally between 75 and 125% of predicted values, to be corrected in the case of anemia or polycythemia). Also defined is the transfer coefficient Kco (= Tlco/ Va = diffusion coefficient = efficiency of one alveolar unit). Interpretation :
- Decreased Tlco and normal (or increased) Kco:
- Pneumonectomy, atelectasis, post-pneumonia or tuberculosis scarring, sarcoidosis, certain non-specific interstitial lung diseases,...
- Obesity, thoracic deformities, pleural effusions, etc.
- Reduced Tlco and Kco (often below 60%): in cases of alveolar or pulmonary vascular damage, or secondary to heart disease or diffuse parenchymal pathologies
- Cryptogenic alveolar fibrosis, pneumoconiosis, infiltrative connectivitis, extrinsic allergic alveolitis, etc.
- Primary pulmonary hypertension, hepato-pulmonary syndrome, arteriovenous malformations, vasculitis
- Pulmonary venous hypertension, pulmonary edema, Eisenmenger's syndrome
- Emphysema, bronchiectasis
- In asthma, Tlco and Kco are normal
- Tlco and Kco are increased in cases of increased perfusion (high cardiac output) or alveolar hemorrhage (Wegener's, Goodpasture's, systemic lupus erythematosus, etc.).
Assessing ventilation control
Under normal conditions, the sum of PaCO2 + PaO2 = 130 +- 5 mmHg. In the event of hypoxemia, the following will usually be observed:
- No change in case of hypoventilation
- Decreased sum in case of intrinsic lung damage (disproportionately severe hypoxemia)
In the event of values that cannot be explained by the pathologies identified, hypercapnia or induced hypoxia tests can be performed.
Respiratory function tests during exercise
Indications:
- Exercise-induced dyspnea with normal cardiorespiratory tuning at rest
- Assessment of training level (incapacitation: contraindication to heavy work if VO2max < 25 ml/kg/min or very heavy work if < 32 ml/ kg/ minute, etc.)
- Assessment of surgical risk (VO2max < 10 ml/ kg/ minute formally contraindicates all thoracic surgery).
- Assessment of treatment or revalidation efficacy
- Suspicion of exercise-induced asthma
Some data :
- VO2 = O2 consumption, VCO2 = CO2 production, VCO2/ VO2 = respiratory quotient
- Ventilatory threshold = anaerobic threshold = breakpoint in respiratory quotient and ventilation/min curves (linear increase up to threshold), expressed as % of VO2max
- StcO2 = O2 saturation of Hb
- ERCO = respiratory equivalent of CO2 (N: 29.1 +- 4.3)
- Predicted maximum heart rate (HR) = 220 - age
Interpretation of maximum VO2: a VO2max < 80% of the predicted value indicates a reduction in physical capacity through
- Under-training: no cardiorespiratory limitation, no reduction in StcO2 and anaerobic threshold < 50% of VO2max
- Respiratory pathology: maximum HR not reached, anaerobic threshold often not reached, ERCO > 35, possible decrease in StcO2 (emphysema, fibrosis,...)
- Cardiac pathology: maximum HR rapidly reached, no respiratory limitation (ventilatory reserve preserved = RV > 30%), anaerobic threshold < 50%, possible drop in StcO2
Exercise-induced asthma is likely if FEV1 decreases by more than 10% at 1, 5, 10, 15 or 30 minutes after exercise (80% of predicted maximum HR reached in 4 minutes).
Bibliography
Gibson GJ, Clinical tests of respiratory function, CRC press, 2008
Kaminsky DA, Overview of pulmonary function testing in adults, Uptodate, Aug 2023
Leslie KO et al., Practical Pulmonary Pathology: A Diagnostic Approach, Elsevier, 2022
Pocock et al., Physiologie humaine, Masson, 2004

