Lyme disease - borreliosis
Lyme disease or borreliosis is an infectious disease with polymorphous manifestations caused by Borrelia (burgdorferi, afzelii and garinii), bacteria transmitted by ticks.
Its incidence is higher in the eastern United States, Scandinavian and Germanic countries. Risk factors: occupational and leisure activities in the forest, duration of contact with the tick (12 to 24 hours are required for transmission).
Lyme disease is generally benign and self-limiting, but its severity depends on the occurrence and severity of joint, cardiac and/or neurological complications.
Its neurological effects (neuroborreliosis) are also dealt with in a separate chapter.
Clinical features
The most frequent manifestations of Lyme disease are cutaneous and articular. More rarely, in ≈ 10% of cases, cardiac and/or neurological disorders are encountered.
Primary phase (3 to 30 days after the bite)

Early and localized :
- Erythema migrans beginning at the bite after 3 to 30 days (80%):
- Erythematous macule or papule progressively transforming into an erythematous annular lesion of low elevation and progressive extension, with - in the majority of cases - a clear central area. The central site of the bite may take on the appearance of a papule, macule, nodule, vesicle or necrotic lesion. This lesion can reach several dozen centimetres in diameter.
- +- Pruritus, burning, pain, satellite adenopathies, systemic signs.
Spontaneous resolution in a few weeks, but may progress to secondary phase.
Secondary phase (3 to 9 weeks after blood-borne bite)

- Skin lesions :
- Multiple erythema migrans with disseminated annular lesions
- Boreal lymphocytoma (firm, smooth pseudotumor nodule) may occur up to 10 months after the bite (1% of adult cases, 7% of pediatric cases), ++ in the ear lobule, nipples and external genitalia +- satellite adenopathies. There are disseminated forms of confluent micro-nodules.
- Acute neuroborreliosis :
- Fever, myalgias, headaches, neck pain, photophobia, confusion.
- Complications: lymphocytic meningitis with cerebrospinal fluid (CSF) composition mimicking viral meningitis, meningoradiculitis (high back pain > asymmetric radiculalgia with or without motor, sensory, reflex or cranial pair involvement (bilateral peripheral facial paralysis is highly suggestive of neuroborreliosis) with predominantly axonal involvement and inflammatory CSF).
- Variable joint involvement: aspecific arthralgias (70%) to chronic, disabling synovitis (rare). Knee arthritis and asymmetric oligoarthritis are highly suggestive.
- Cardiac involvement (4-10% of cases), ++ diffuse transmural inflammatory infiltrate with chest pain, dyspnea, syncope or palpitations +- electrocardiographic abnormalities (++ BAV). Occurrence of left heart failure or valvular lesions is very rare.
Tertiary phase (several months to years after the bite)
The picture is generally centered on a single clinical area (neurological, articular or cutaneous). In Europe, this is most often skin involvement with recurrent chronic migrant erythema, often with pruritus and burning, and chronic atrophic acrodermatitis (cigarette-paper appearance with visible venous network, loss of elasticity and areas of depigmentation and/or desquamation) +- loco-regional adenopathy, asthenia, weight loss, sensory polyneuropathy. Highly suggestive: hyperesthesia to shock of bony protrusions at the site of lesions, damage to underlying joints.
Other presentations are rarer: progressive encephalomyelitis (all central deficits may be encountered, with or without impaired alertness, MRI usually showing lesions of the periventricular white matter that are not very specific, CSF may show hyperproteinorachia and positive serology), late encephalopathy (memory disorders, sleep disorders, irritability, emotional lability, depression).
What about "post-borreliosis syndrome" or "chronic borreliosis"?
Post-borreliosis syndrome is defined by a documented history of borreliosis, treated with appropriate antibiotic therapy, absence of serological evidence of reinfection, exclusion of differential diagnoses, and persistence of symptoms possibly associated with aspecific complaints (fatigue, arthromyalgia, difficulty concentrating, etc.) in the absence of objective signs. It is sometimes incorrectly referred to as "chronic borreliosis" (leading to confusion with tertiary phases).
There are no data to support any link between this syndrome and borreliosis. In any case, antibiotic treatment in this situation is not recommended.
Diagnosis
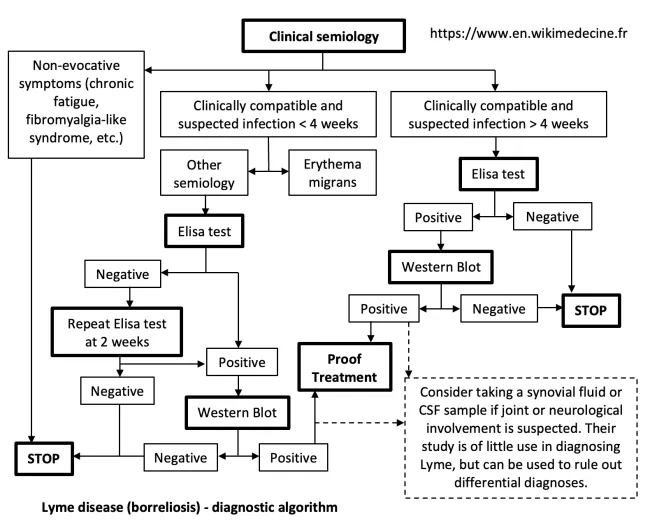
- Anamnesis: risk behavior, tick bite, compatible complaints
- Clinical: see above, the clinic is the main diagnostic factor. Typical erythema migrans is sufficient for diagnosis (serologies at this stage are in any case unreliable).
- Blood serology (Ig M becomes negative in 3 to 6 months):
- Elisa test (highly sensitive, negative predictive value > 99% even for high-prevalence groups) - sometimes negative in the first 3 weeks of infection.
- If positive → Western Blot test for confirmation
- Serology poses two problems:
- In the primary phase, the false-negative rate is high. Diagnosis then depends essentially on clinical findings.
- In the tertiary phase, IgM is generally negative. IgG positivity alone cannot distinguish between a true positive and a simple serological scar indicating past exposure (these false positives represent up to 10% of the population in areas of high prevalence). What's more, the tests also recognize other spirochetes (false positives). In short, serological tests can reasonably exclude the disease, but cannot confirm it with certainty. They should therefore only be carried out on the basis of a reasonable pre-test clinical probability.
- Elisa test (highly sensitive, negative predictive value > 99% even for high-prevalence groups) - sometimes negative in the first 3 weeks of infection.
- In the event of positive blood serologies, examination (with serologies) of synovial or cerebrospinal fluids is recommended in cases of suspected joint or neurological involvement. However, the only specific anomaly is an index of Ig borrelia in relation to blood > 2, but this is not very sensitive. However, these tests can help exclude certain differential diagnoses.
- Biopsies of lesions with histology and PCR (skin, CSF, urine, synovial fluid, blood): low sensitivity, high cost → not recommended.
In summary:
- Aspecific symptoms (chronic fatigue, "fibromyalgia-like" syndrome) → stop
- Suspicion of infection (compatible objective sign) less than 4 weeks old :
- Erythema migrans → diagnosis of probable Lyme → treat
- Other manifestations → blood serologies
- positive → diagnosis of Lyme possible to probable → trial treatment
- negative → repeat blood serologies in 2 weeks
- positive → diagnosis of Lyme possible to probable → test treatment
- negative → stop
- Suspicion of infection (compatible objective sign - or suggestive symptom lasting more than three weeks) of > 4 weeks → perform blood serologies
- Negative Elisa test → stop
- Elisa test positive → perform Western Blot
- Negative Western Blot → stop
- Western Blot positive → diagnosis of Lyme possible to probable → trial treatment
Therapeutic management - Treatments
Example of therapeutic plan:
- For isolated erythema migrans → amoxicillin 3 x 500 mg/day or doxycycline 2 x 100 mg/day PO for > 2 weeks
- Rapid or severe articular, cardiac or neurological forms → consider treatment with ceftriaxone 1 x 2 g/day IV for a minimum of 3 weeks (inpatient or "day hospital")
Tick bite prophylaxis
No systematic prophylaxis is recommended for tick bites. A single 200 mg dose of doxycycline may be considered if a tick is removed after 24 hours in a highly endemic region.
Bibliography
Hu L, Clinical manifestations of Lyme disease in adults, UpToDate, 2023
Hu L, Diagnosis of Lyme disease, 2023
Hu L, Treatment of Lyme disease, UpToDate, 2023
Jameson JL et al., Harrison's Principles of Internal Medicine, 20th edition, McGraw Hill Higher Education, 2018
Maladies infectieuses. Attitudes pratiques, diagnostiques et thérapeutiques, Hôpital Erasme, 2016
Mead P, Epidemiology of Lyme disease, UpToDate, 2021Traité d'infectiologie, Encyclopédie médico-chirurgicale, Elsevier, 2014