Neuroborreliosis (neurological effects of Lyme disease)
Neuroborreliosis is defined as the neurological manifestations of Lyme disease (general and extra-neurological aspects are dealt with in a separate chapter).
Lyme disease or borreliosis is a systemic infection with certain Borrelia (tick-borne spirochetosis) whose manifestations are usually limited to the cutaneous and articular spheres. More rarely (≈ 10% of cases), it is complicated by cardiac and/or neurological manifestations, which make it particularly serious.
As a rule, the early neurological complications of borreliosis have an excellent spontaneous prognosis, whereas late-onset disease usually evolves adversely in absence of treatment.
As the most suggestive cutaneous and articular manifestations of the disease can be frustrating, they are not always found in the patient's clinical history. In addition, neuroborreliosis is highly protean, and very difficult to diagnose in the absence of documented Lyme disease.
Clinical
Neuroborreliosis is highly protean... however, the most classic clinical pictures, isolated or associated, are :
- Early infection (manifestation 1 to 10 weeks after erythema migrans):
- Meningoradiculitis improving spontaneously after a few months. Cerebrospinal fluid analysis usually shows lymphocytic pleocytosis, and conduction velocities show predominant axonal involvement.
- Guillain-Barré syndrome
- Involvement of the cranial pairs (++ nerve VII, bilateral or tilting facial paralysis being highly suggestive) +- radiculopathy
- Meningitis of acute onset ++ paucisymptomatic, cerebrospinal fluid showing pleocytosis ++ 100-200 cells/ cc with hyperproteinorachia, spontaneous resolution in a few months. Isolated headaches without meningitis are common.
- Severe meningoencephalomyelitis or transverse myelitis (++ Th 4 to 10) are rare.
- Myositis
- During persistent or late infection :
- European late central neuroborreliosis = progressive encephalomyelitis :
- Very rare (0.3% of infections), ++ chronic or sub-acute presentation, although sudden onset presentations have been described.
- ++ progressive onset of central deficits (all types described, spinal cord signs predominant in 50%), absence of meningeal syndrome or fever.
- Lumbar puncture: cellularity and proteinorachy may be borderline normal... usual presence of oligoclonal bands,orrelia serology may be positive.
- American late central neuroborreliosis = late encephalopathy
- Less severe than the European form, ++ aspecific encephalopathy with asthenia, cognitive and depressive disorders. No focal deficits. May be associated with polyneuropathy.
- Lumbar puncture: variable, inconstant abnormalities... may be strictly normal.
- Cerebral NMR: contrast-enhancing punctiform signals in white matter.
- European late peripheral neuroborreliosis
- Progressive axonal polyneuropathy with paresthesias, often painful, distal ++ asymmetric, asthenia.
- Lumbar puncture: variable and inconstant abnormalities
- Response to antibiotic therapy is generally poor.
- Late American peripheral neuroborreliosis
- Subacute to chronic polyneuropathy.
- Lumbar puncture: variable and inconstant abnormalities.
- "Post-borreliosis syndrome"
- This is defined by a documented history of borreliosis, treated with appropriate antibiotic therapy, absence of serological evidence of reinfection, exclusion of differential diagnoses and persistence of symptoms + asthenia, arthromyalgia, concentration difficulties. Its biological substrate is debated: functional origin? No EBM on possible management.
- European late central neuroborreliosis = progressive encephalomyelitis :
Diagnosis
Clinical diagnosis is straightforward in the early stages, when skin involvement is suggestive. However, neuroborreliosis without cutaneous involvement (or undetected) is possible → also to be suspected in the presence of lymphocytic meningitis, meningoradiculoneuritis, facial neuropathy, acute or chronic (encephalo)-myelitis and chronic polyneuropathies of undetermined origin. Only a third of patients reported having been bitten by a tick.
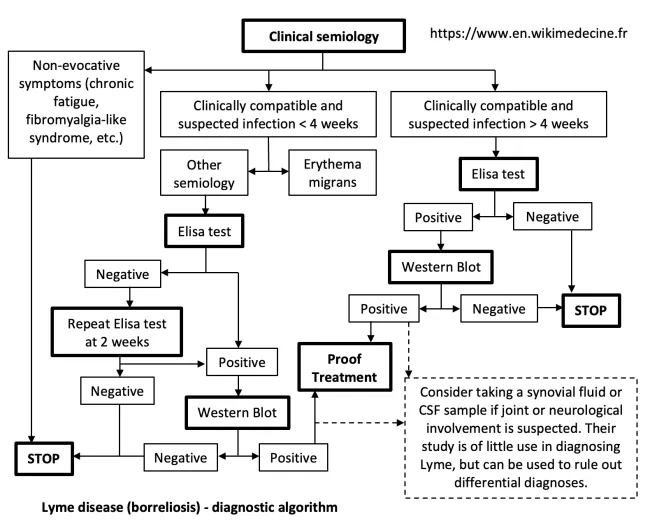
Biological diagnosis: ELISA serology → Western Blot (highly specific) if ELISA positive or borderline. Very good sensitivity of ELISA in late stage... but mediocre in early → to be repeated in case of reasonable clinical presumption at 2 or 3 weeks.
Cerebrospinal fluid may show aspecific abnormalities (lymphocytic meningitis,...). Intrathecal anti-borrelia antibody synthesis (index > 2) confirms the diagnosis, but its absence does not rule it out.
→ Early-stage serological diagnosis is straightforward (Ig G and Ig M positive). In the persistent or late stage (Ig G positive and Ig M negative), it is impossible to differentiate between an incidentaloma (simple "serological scar) and true neuroborreliosis → current consensus = in case of clinical suspicion (objectivable abnormalities, suggestive of pathology and with no best explanation), consider empirical trial antibiotic therapy.
On the other hand, some series report up to 7% of neuroborreliosis cases with persistent negative serology → some recommend empirical trial therapy in cases of strong clinical suspicion, with response to antibiotic therapy being a strong diagnostic argument. It should be noted that there is no EBM for such an attitude, which, depending on the appropriateness of its clinical judgment, opens the door to many abuses. It should therefore only be considered in exceptional cases.
Therapeutic management - Treatments
If neurological damage is present, treatment is generally started in hospital (or in a day hospital) with ceftriaxone IV 1 x 2 g/day ++ for > 3 weeks (minimum 2). Possible Jarisch-Herxheimer reaction (fever, myalgias, headaches, tachycardia, hypotension, worsening of neurological lesions... appearing under treatment - to be treated symptomatically with anti-inflammatories and/or corticoids). Alternative: pen G 20 MU/ day IV.
In the case of discrete, slowly evolving symptoms, outpatient treatment (amoxicillin 3 x 500 mg/day or doxycycline 2 x 100 mg/day PO for > 2 weeks) may be considered.
Bibliography
Bradley WG et al., Neurology in clinical practice, Elsevier, 2021
Goetz GC, Textbook of Clinical Neurology, Elsevier, 2007
Halperin JJ, Nervous system Lyme disease, UpToDate, 2021
Jameson JL et al., Harrison's Principles of Internal Medicine, 20th edition, McGraw Hill Higher Education, 2018
Maladies infectieuses. Attitudes pratiques, diagnostiques et thérapeutiques, Hôpital Erasme, 2016
Traité de Neurologie, Encyclopédie médico-chirurgicale, Elsevier, 2014